
Professor in Pathology
Associate Professor of Biomedical Engineering
Associate Professor in Integrative Immunobiology
Member of the Duke Cancer Institute
📞 919-681-0815
Overview
Our lab focuses on mechanisms of T-cell dysfunction in the context of central nervous system tumors, including T-cell exhaustion and sequestration. This strong immunologic foundation serves as the basis for our active development of cell and biologic therapeutics, including chimeric antigen receptor (CAR) T-cells and T-cell and antigen bispecifics (TCABs). We are further currently modeling cutting-edge neurosurgical therapies (“bedside to bench”) alongside colleagues in biomedical engineering and veterinary medicine. Our team is comprised of a unique mix of scientists, clinicians, and students working to improve the care of patients with brain tumors.
Our Research
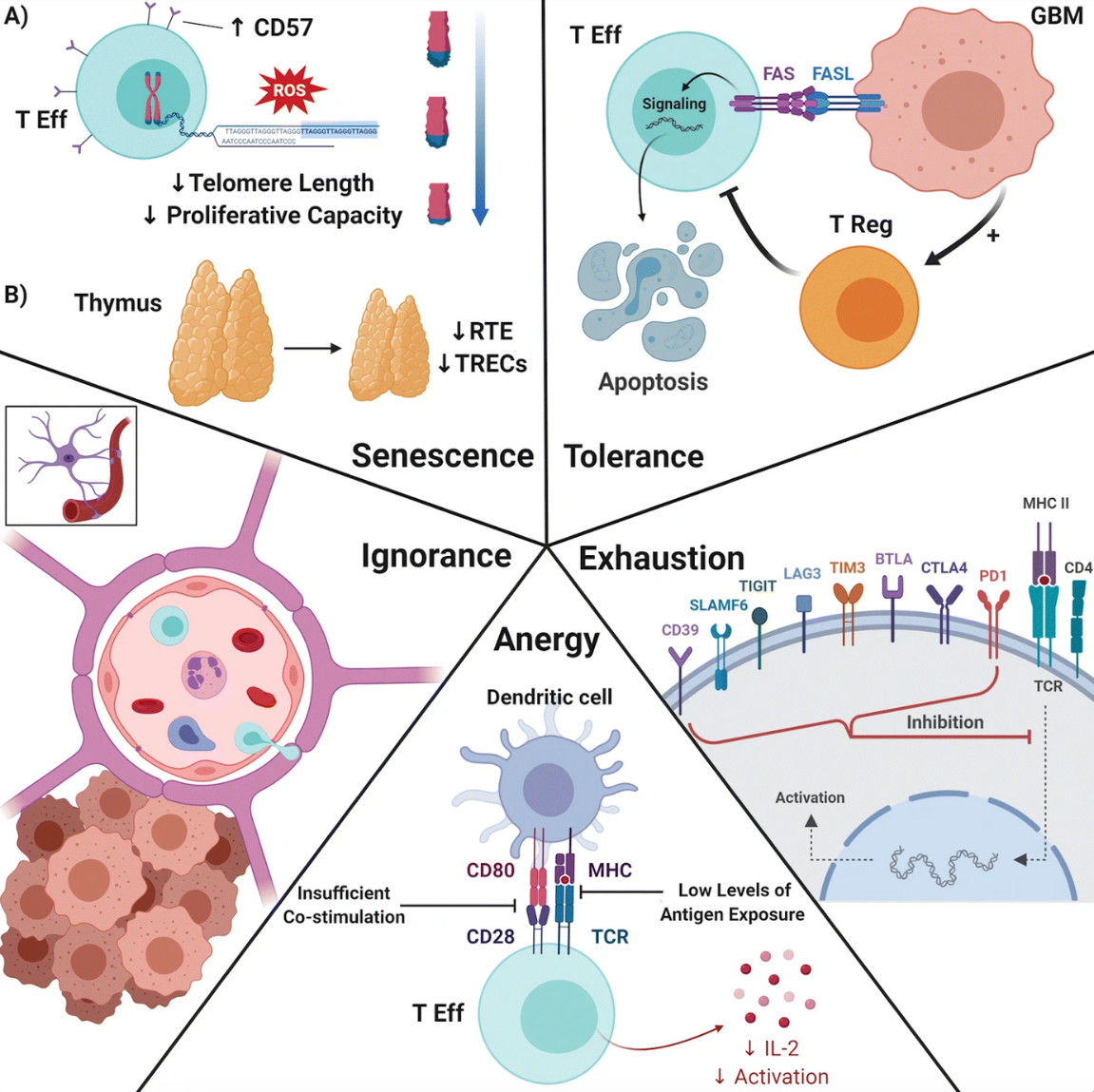
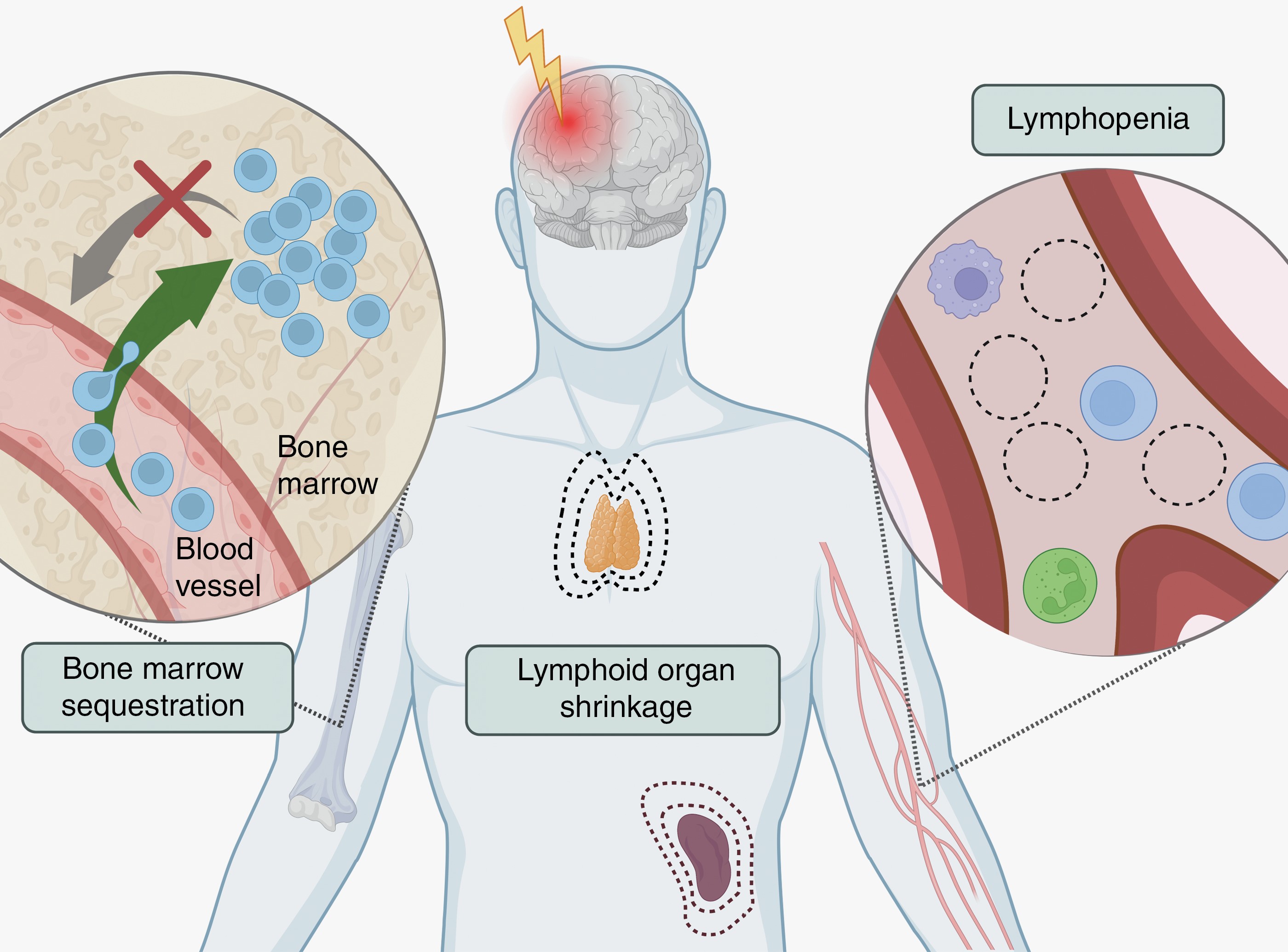
T-cell dysfunction in central nervous system malignancies
Historical notions of the brain as an inert, immunologically-privileged compartment have given way to an understanding of the brain as immunologically distinct. Our lab studies the unique mechanisms by which T-cell dysfunction arises in primary and metastatic brain tumors, including T-cell sequestration in the bone marrow and T-cell exhaustion within the tumor-immune microenvironment. We additionally recently discovered a novel mechanism by which T-cells can kill tumor cells in the absence of antigen presentation on MHC-I. We are currently working to further our understanding of T-cell exhaustion and identify the mechanism by which brain-specific T-cell sequestration occurs.
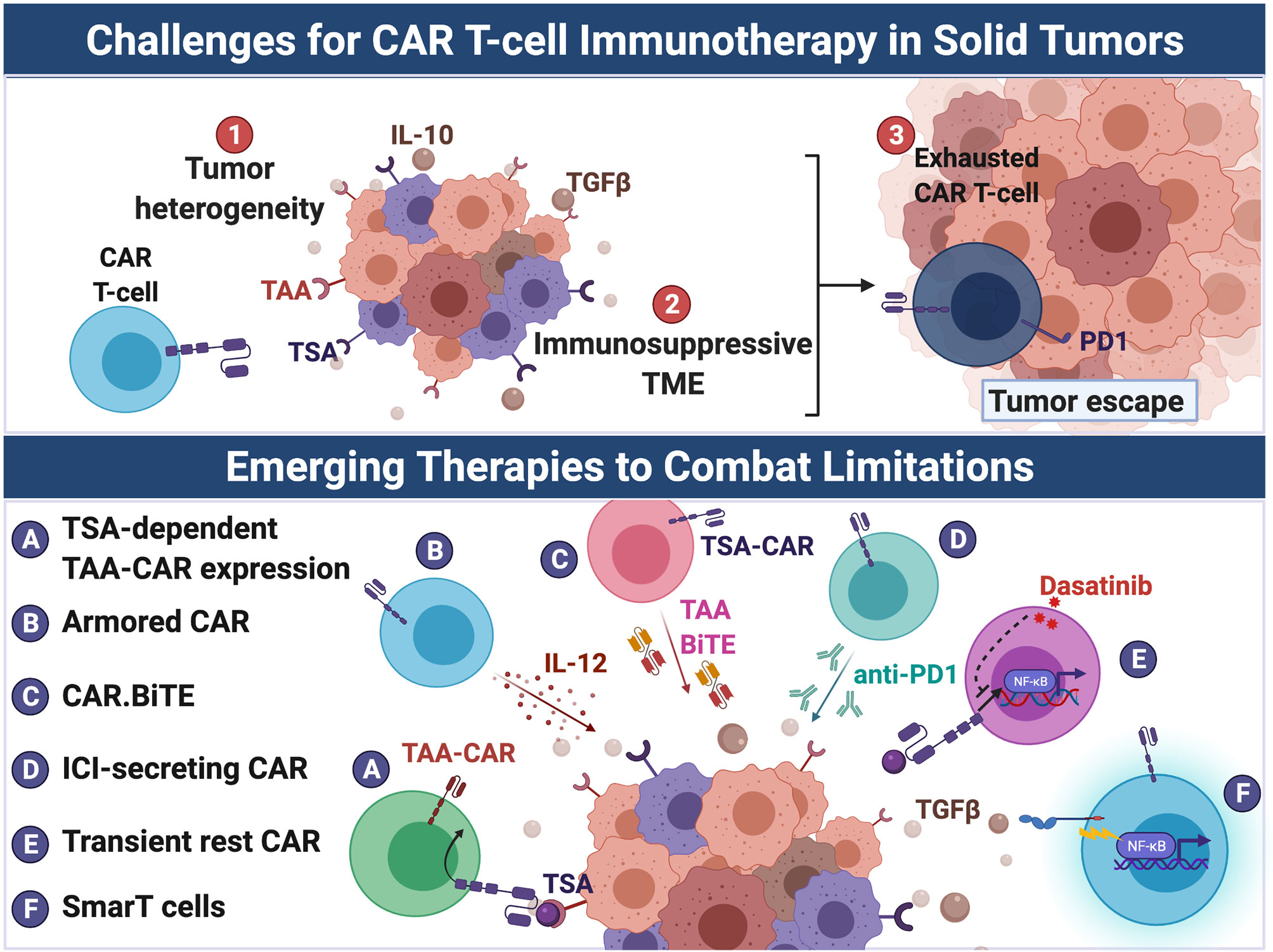
CARs and TCABs
As an extension of our work on T-cell dysfunction, we are interested in developing cell-based therapies for CNS tumors, including chimeric antigen receptor (CAR)-T cells and T-cell and antigen bispecifics (TCABs). Together with Dr. Anoop Patel, we are leveraging immunogenomic techniques to streamline the development and translation of these therapies to the clinic. Several investigators share mentorship and resources between the Fecci and Patel labs as part of our collaborative program, LOgic-Gated Immune and Synthetic Therapies for Intracranial Cancers (LOGISTIC).
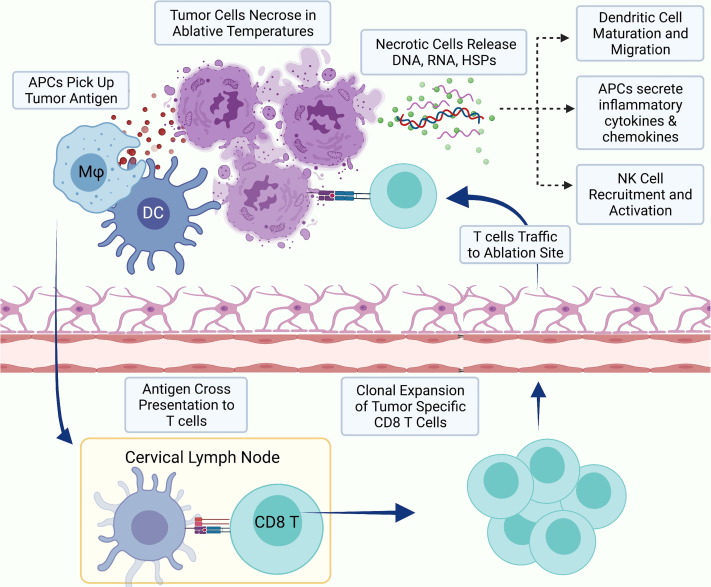
Nanotechnologies and LITT
Laser interstitial thermal therapy (LITT) is a novel, minimally invasive treatment for primary and metastatic brain tumors that is currently in clinical use. Given a wealth of evidence on the ability of hyperthermia to induce mechanisms of innate and adaptive antitumor immunity, our lab is interested in leveraging LITT as a platform for in situ vaccination in combination with systemic immunotherapies. We recently partnered with the Department of Biomedical Engineering to develop tumor-selective gold nanostars that enable greater and more precise hyperthermia. We are currently studying the immunology of LITT in both murine models and companion animals being treated for spontaneously arising gliomas, in collaboration with the NC State College of Veterinary Medicine.
Selected Publications
- Lerner EC, Woroniecka KI, D'Anniballe VM, et al. CD8+ T cells maintain killing of MHC-I-negative tumor cells through the NKG2D-NKG2DL axis. Nat Cancer. 2023;4(9):1258-1272. doi:10.1038/s43018-023-00600-4
- Srinivasan ES, Liu Y, Odion RA, et al. Gold Nanostars Obviate Limitations to Laser Interstitial Thermal Therapy (LITT) for the Treatment of Intracranial Tumors. Clin Cancer Res. 2023;29(16):3214-3224. doi:10.1158/1078-0432.CCR-22-1871
- Lorrey SJ, Waibl Polania J, Wachsmuth LP, et al. Systemic immune derangements are shared across various CNS pathologies and reflect novel mechanisms of immune privilege. Neurooncol Adv. 2023;5(1):vdad035. Published 2023 Apr 11. doi:10.1093/noajnl/vdad035
- Lerner EC, Edwards RM, Wilkinson DS, Fecci PE. Laser ablation: Heating up the anti-tumor response in the intracranial compartment. Adv Drug Deliv Rev. 2022;185:114311. doi:10.1016/j.addr.2022.114311
- Waibl Polania J, Lerner EC, Wilkinson DS, Hoyt-Miggelbrink A, Fecci PE. Pushing Past the Blockade: Advancements in T Cell-Based Cancer Immunotherapies. Front Immunol. 2021;12:777073. Published 2021 Nov 18. doi:10.3389/fimmu.2021.777073
- Miggelbrink AM, Jackson JD, Lorrey SJ, et al. CD4 T-Cell Exhaustion: Does It Exist and What Are Its Roles in Cancer?. Clin Cancer Res. 2021;27(21):5742-5752. doi:10.1158/1078-0432.CCR-21-0206
- Grabowski MM, Sankey EW, Ryan KJ, et al. Immune suppression in gliomas. J Neurooncol. 2021;151(1):3-12. doi:10.1007/s11060-020-03483-y
- Srinivasan ES, Sankey EW, Grabowski MM, Chongsathidkiet P, Fecci PE. The intersection between immunotherapy and laser interstitial thermal therapy: a multipronged future of neuro-oncology. Int J Hyperthermia. 2020;37(2):27-34. doi:10.1080/02656736.2020.1746413
- Woroniecka KI, Rhodin KE, Dechant C, et al. 4-1BB Agonism Averts TIL Exhaustion and Licenses PD-1 Blockade in Glioblastoma and Other Intracranial Cancers. Clin Cancer Res. 2020;26(6):1349-1358. doi:10.1158/1078-0432.CCR-19-1068
- Kemeny HR, Elsamadicy AA, Farber SH, et al. Targeting PD-L1 Initiates Effective Antitumor Immunity in a Murine Model of Cushing Disease. Clin Cancer Res. 2020;26(5):1141-1151. doi:10.1158/1078-0432.CCR-18-3486
- Liu Y, Chongsathidkiet P, Crawford BM, et al. Plasmonic gold nanostar-mediated photothermal immunotherapy for brain tumor ablation and immunologic memory. Immunotherapy. 2019;11(15):1293-1302. doi:10.2217/imt-2019-0023
- Chongsathidkiet P, Jackson C, Koyama S, et al. Sequestration of T cells in bone marrow in the setting of glioblastoma and other intracranial tumors. Nat Med. 2018;24(9):1459-1468. doi:10.1038/s41591-018-0135-2
Patents
- Tim-4 Bi-Specific T Cell Engager (BiTE) And Chimeric Antigen Receptor (CAR) T Cell Delivery System And Methods Of Making And Using Same, Atty Docket No.: DU7805PROV (Provisional)
- Nanoplasmonics-Enhanced Laser Interstitial Thermal Therapy Systems And Methods Thereof, US Provisional Patent Application #63/213,928
- Chimeric Apoptotic Signal Targeting Lymphocytes (Tim-4 Castl) And Methods Of Making And Using Same, Atty Docket No.: DU7046PROV (Provisional), (Filed 11/2/2021)
- “D2C7 EGFR And EGFR RVIII Bi-Specific Chimeric Antigen Receptor Contructs And Methods Of Making And Using Same”, US Application # 63/217,399 (Filed 7/1/2021)
- Compositions and Methods for the Treatment of Intracranial Disease”, US Applications # 62/881,486 and # 62/885,514 (Filed 8/1/2019 and 8/12/2019)
- “Enhanced Immunological Responses”, US Application # 13/336,590 (Filed 12/23/2011)
- “Trimodal Cancer Therapy”, US Application # 61/261,476 (Conceived 3/2/2006)
Grants
Current
i. Lloyd J. Old STAR Award, Cancer Research Institute: Removing barriers to immunotherapy against tumors within the intracranial compartment. Fecci (PI), 07/01/21 – 06/30/26
ii. 5P50-CA190991-08 , NIH/NCI Brain SPORE: Project 2: "Arresting” bone marrow T cell sequestration in GBM. Fecci/Lefkowitz (Project Co-Leads), 09/01/19 – 08/31/24.
iii. 2R25-NS065731-11A1, NIH: Research Education Programs for Residents and Fellows in Neurosurgery. Fecci (Co-PI), 09/01/19 – 08/31/24.
iv. 1R01-CA257009-01A1, UNC-CH/NIH: Tunable Temporal Drug Release for Optimized Synergistic Combination Therapy of Glioblastoma. Fecci (Site PI), 07/01/21 – 06/30/26.
v. Duke Health Scholars Award. Fecci (PI), 11/18/16 – Present
vi. 1R01-FD007283-01, NIH/FDA: Phase 2 trial of a novel peptide vaccine targeting CMV antigen for newly diagnosed pediatric high grade glioma and diffuse intrinsic pontine glioma and recurrent medulloblastoma. Thompson (PI), Fecci (Investigator), 09/20/21 – 08/31/25.
vii. Monteris Medical, Inc., REMASTer Trial. Fecci, (PI) 11/11/21 – 12/31/26.
Personnel
Peter E. Fecci, MD, PhD
Principal Investigator
Professor of Neurosurgery
Professor in Pathology
Associate Professor in Integrative Immunobiology
Associate Professor of Biomedical Engineering
Member of the Duke Cancer Institute
Director, Neurosurgical Oncology
Director, Duke Center for Brain and Spine Metastasis
As the director of the Brain Tumor Immunotherapy Program, Surgical Neuro-Oncology, and the Center for Brain and Spine Metastasis at Duke University, I focus our programmatic interests on the design, optimization, and monitoring of immune-based treatment platforms for patients with intracranial tumors, whether primary or metastatic. Within this broad scope, however, my own group looks more specifically at limitations to immunotherapeutic success, with a particular focus on understanding and reversing T cell dysfunction in patients with glioblastoma (GBM) and brain metastases. I very much look to collaboratively integrate our approaches with others investigating innovative treatment options. I continue my focus on combining strategies for reversing T cell deficits with current and novel immune-based platforms as a means of deriving and improving rational and precise anti-tumor therapies. It is my sincerest desire to forge a career focused on co-operative, multi-disciplinary, organized brain tumor therapy. Ultimately, my goal is to help coordinate the efforts of a streamlined and effective center for brain tumor research and clinical care. I hope to play some role in ushering in a period where the science and treatment arms of brain tumor therapy suffer no disjoint, but instead represent the convergent efforts of researchers, neuro-oncologists, medical oncologists, radiation oncologists, biomedical engineers, and neurosurgeons alike. I hope to see such synergy become standard of care.
Current Staff
Xiuyu Cui, MS - Associate in Research
Xiuyu has over 25 years working in both clinical and pre-clinical research at Duke. She earned her BS in Biology at Beijing Normal University and MS in Forestry at University of Maine. She currently helps run the Longitudinal Assessment of Marrow and Blood in patients with Glioblastoma (LAMB-G) study, and maintains our repertoire of mouse models, assays, and experimental procedures for internal and external collaborations. Her outside interests include traveling, cooking, gardening, and spending time with family and dogs (Romeo and Ace).
David Snyder BS, LATG – Research Analyst II
Dave manages the animal colony for pre-clinical studies, writes animal research protocols and trains students in lab animal research techniques. He earned bachelor’s degrees in Biology and Veterinary Technology at Mt. St Vincent and Mercy College, and is AALAS certified. His outside interests include performing 18th Century living history, hunting, fishing, wildlife photography and kayaking.
Daniel Wilkinson, PhD – Senior Research Associate (LOGISTIC Investigator)
Dan is a former Fecci Lab post-doc and current staff scientist. His project focuses on the rational design and engineering of novel T cell-based therapies for solid tumors. While this research is primarily preclinical, the ultimate goal is to translate these therapies into clinical trials. He completed his BS at UNC-Chapel Hill and PhD in Microbiology and Immunology at ECU. Outside of lab, he enjoys movies, video games, and spending time with his cats.
Clinical Fellows
Andrew Hardigan, MD, PhD – Neurosurgery Resident (LOGISTIC Investigator)
Joshua Jackson, MD, PhD – Neurosurgery Resident
Josh’s primary research interest involves the study interferon signaling and how this influences the immunobiology of glioblastoma and how this network can be modulated for therapeutic effect. He anticipates a career as a neurosurgeon-scientist bridging the gap between the historic treatment paradigm for glioblastoma and the uncovering advances which will enable longer survival and a diminished role for surgery in the future. He completed his MD and PhD at the University of Alabama, Birmingham following undergraduate work in chemical engineering. Beyond the lab, he enjoys college football, professional hockey, and spending time outdoors including gardening, hiking and caving.
Graduate Students
Selena Lorrey, BA – Graduate Student, Integrative Immunobiology
Selena’s PhD research is focused on understanding the challenges to immunotherapeutic success that are specific to brain cancer. In particular, her work is focused on understanding the systemic immunosuppression that arises from brain tumors and designing rational interventions to overcome this challenge and license the use of immunotherapy. She earned her Bachelor’s degree at Bowdoin College and outside of lab, she enjoys cooking, reading, lifting, and travel!
Luke Wachsmuth, BS – MSTP Student, Pathology
Luke’s PhD research focuses on characterizing the mechanism of systemic immune derangements in both brain tumors and other CNS paothologies. He has an extensive background in immunology from his time as a NIH Post-Bac and his undergraduate work at the University of Georgia. Outside of lab, he enjoys cooking from the New York Times, hiking/camping, and gardening.
Xanne Hoyt-Miggelbrink, MD – Graduate Student, Pathology
In Xanne’s current project, she has identified a novel marker of exhaustion that has implications for both the upregulation of the exhaustion program as well as anti-tumor immunity. After she graduates, she plans to do a postdoc in Dr. Ayasoufi's lab at Duke.She is originally from the Netherlands and completed her MD at the University of Utrecht and BS at the University of Leiden prior to arriving at Duke. Outside of lab, she likes to go rock climbing, watch sports, and read books.
Olivia Balmert, BS – Graduate Student, Integrative Immunobiology
Olivia’s project explores the changes in bone marrow hematopoiesis that occur in the context of intracranial tumors, and how these changes impact the constitution of the tumor microenvironment and the immune system’s ability to mount an anti-tumor response. After graduation she hopes to work in industry doing translational research. She originally completed her BS at the University of Notre Dame. Outside of the lab, she enjoys cooking, gardening, and listening to audiobooks.
Emily Lerner, MHS – MSTP Student, Biomedical Engineering
Emily recently uncovered a novel mechanism of MCH-I independent tumor cell killing and now focuses on immune engineering cell-based therapies. After graduation, she plans to pursue residency. She is a skilled glass blower and recently presented her pieces at a gallery showing!
Kirit Singh, MBBS – Graduate Student, Biomedical Engineering
Kirit Singh is a biomedical engineering PhD candidate and a Preparing Future Faculty fellow. His research focuses on translational drug development (primarily TCABs) and surgical window of opportunity trials. He originally completed his MBBS at Barts and the London in the UK and hopes to pursue residency in neurosurgery following his PhD.
Bhairavy Puviindran, BS – Graduate Student, Biomedical Engineering
Bhairavy recently joined the Fecci lab in 2023 after completing her BS in Biomedical Engineering at NC State and Post-Bac at the NIH, where she worked on focused ultrasound. She hopes to build on previous Fecci Lab findings to understand why local and systemic immunosuppression occur. Upon graduating, she hopes to pursue a career in industry. Outside of lab, she loves to cook/bake, dance (Bharathanatyam), and tend to her succulents!
Shannon Wallace, BS - Graduate Student, Biomedical Engineering
Aditya Mohan, BS – MSTP Student, Biomedical Engineering (LOGISTIC Investigator)
Medical Students
Aden Haskell-Mendoza, MS
Aden is a third year medical student at Duke conducting a two-year research project on the immunology of LITT in the Fecci lab. He completed his MS in Biology and BS in Neuroscience at UC San Diego, where he worked in the labs of Drs. Jean Wang and Clark Chen to investigate radiation-induced bystander and abscopal effects in glioblastoma. In between medical school and undergrad, he helped initiate a brain tumor immune monitoring program at UC Davis with Orin Bloch, MD. Outside of lab, he enjoys the Sacramento Kings, music production/audio engineering, fitness, and finding the best restaurants in the Triangle with his fiancée.
Collaborators
- Robert Lefkowitz, MD, Department of Medicine, Duke University
- Lindsay Rein, MD, Department of Medicine, Duke University
- Anoop Patel, MD, Department of Neurosurgery, Duke University
- Simon Gregory, PhD, Department of Neurosurgery, Duke University
- Katayoun Ayasoufi, PhD, Department of Neurosurgery, Duke University
- Michael Dee Gunn, MD, Department of Medicine, Department of Integrative Immunobiology, Duke University
- Carey Anders, MD, Department of Medicine, Duke University
- Chris Mariani, DVM, Ph, Veterinary Neurology and Neurosurgery, North Carolina State School of Veterinary Medicine
- Alem Kahsai, PhD, Department of Medicine, Duke University
- Michelle Monje, MD, PhD, Stanford Medicine
- Kyle Walsh, PhD, Department of Neurosurgery, Duke University
- Tuan Vo-Dinh, PhD, Department of Biomedical Engineering, Duke University
- David Ashley, MBBS, PhD, Department of Medicine, Department of Neurosurgery, Duke University
- Anne Marie Pendergast, PhD, Deparment of Pharmacology and Cancer Biology, Duke University
- Dorothy Sipkins, MD, PhD, Department of Medicine, Duke University
- John H. Sampson, MD, PhD, Department of Neurosurgery, Duke University
Lab Alumni
- Jessica Waibl-Polania, PhD; Pathology Graduate Student, 2018-2024: AbbVie, Inc., South San Francisco, CA
- Joseph “Zach” Wilson, MD; Post-Doc, 2021-2023: Pediatric Neuro-Oncology Fellow, Duke University
- Ryan Edwards, MD; Medical Student, 2020-2022: Internal Medicine Resident, Duke University
- David Huie, MD; Post-Doc, 2020-2021: Neurosurgery Fellow, Duke University
- Pakawat Chongsathidkiet, MD, PhD; Graduate Student/Post-Doc 2015 – 2021: Neurosurgery Resident, Duke University.
- Eric Sankey, MD; Post-Doc, 2019-2021: Staff, Piedmont Athens Neurosurgery
- Matthew Grabowski, MD; Post-Doc, 2019-2020: Neurosurgeon, Cleveland Clinic
- Katherine Ryan, DO; Post-Doc, 2019-2021: Assistant Professor, Stanford University
- Ethan Srinivasan, MD; Medical Student, 2019-21: Neurosurgery Resident, Johns Hopkins University
- Cosette Champion, MD; Medical Student, 2017-19: Internal Medicine Chief Resident, Washington University in St. Louis
- Kristen Rhodin, MD: Medical Student, 2017-18: General Surgery Resident, Duke University
- Hanna Kemeny, MD: Medical Student, 2017-18: Neurosurgery Resident, Northwestern University
- Vadim Tsvankin, MD: Post-Doc, 2016-17: Director of Neurosurgical Oncology, Colorado Brain and Spine Institute
- Karolina Woroniecka, MD, PhD; Graduate Student, 2016 -2019: WPM Pathology Laboratory
- John Berry-Candelario, MD, MPH; Post-Doc, 2015-2016: Staff, Novant Health Spine Specialists
- Aladine Elsamadicy, MD; Medical Student, 2015-2017: Neurosurgery Resident, Yale University
- Harrison Farber, MD; Medical Student, 2014-2016: Neurosurgery Resident, Barrow Neurological Institute
Join Us
Our Lab Culture
The Fecci lab is built upon the following five strategic pillars:
1) scientific rigor
2) mentorship
3) community
4) ethical behavior
5) open collaboration
The group is strongly committed to diversity and inclusion and provides a supportive environment that upholds the common goal of promoting equitably derived scientific research. Our collective success depends on our ability to work together and to trust and empower each other to become creative thinkers who contribute to expanding scientific knowledge, as well as to improving outcomes for patients with cancer. Our goal is to produce thought leaders who are respected by the scientific community based on their evident embodiment of both excellence and citizenship.
If you are interested in joining or would like to see if the lab is a good fit, please reach out to Marissa Bianchi, Administrative Assistant to Dr. Fecci at marissa.bianchi@duke.edu.
